
Canada lands high on list of world's most relaxing destinations
When you think of relaxing destinations, you probably picture white sandy beaches and warm waters, which aren't usually associated with Canada.
Turns out that the True North ranks as one of the top destinations in the world for some R&R, according to BookRetreats' newly published Holiday Relaxation Report.
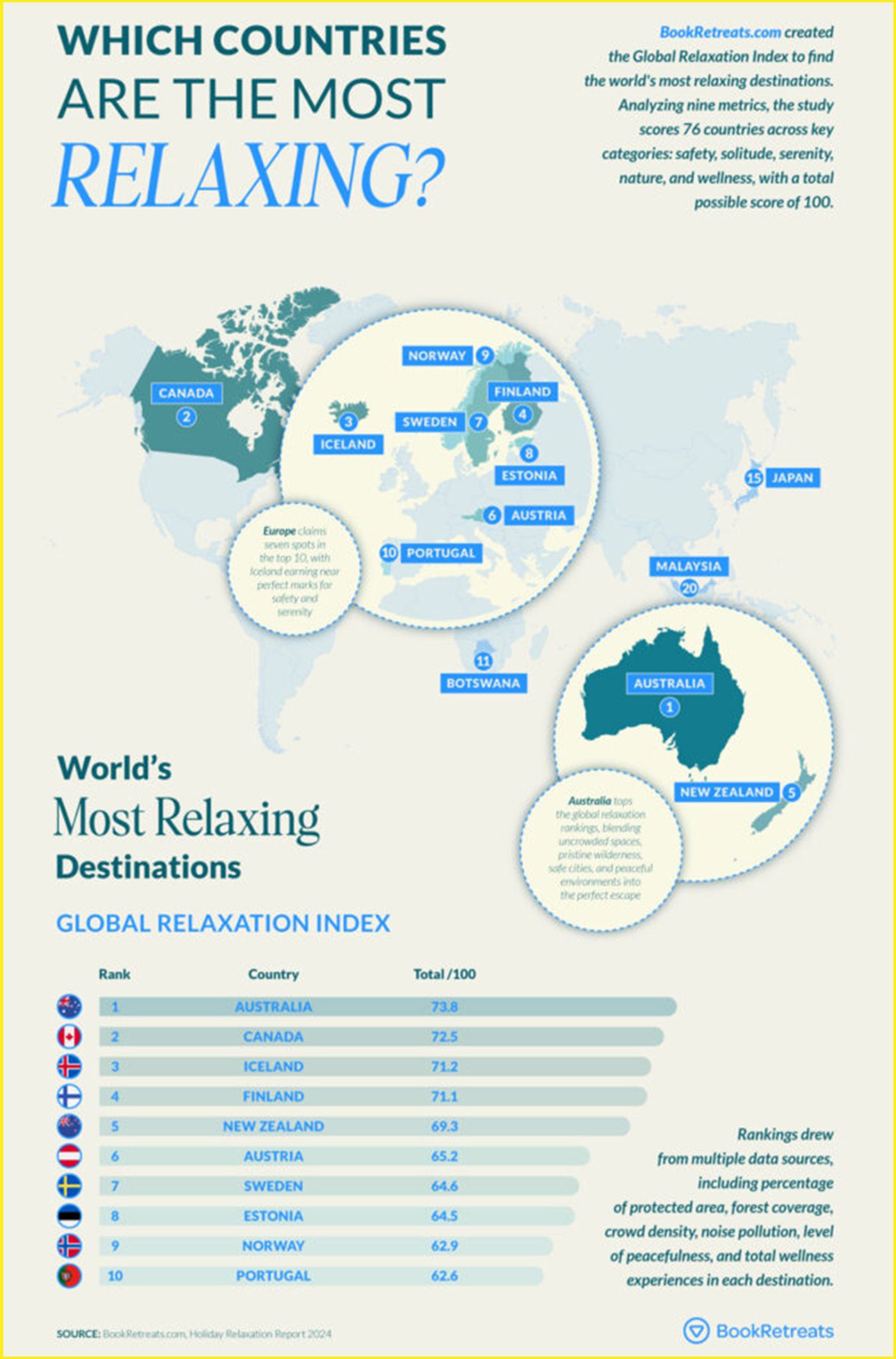
The travel experience website examined 76 destinations and ranked each place based on five factors: safety, solitude, serenity, nature and wellness. Each criterion was weighted differently.
Under these criteria, BookRetreats took into account several data points (percentage of protected area, forest coverage, crowd density, noise and light pollution, peacefulness, and total wellness experiences). Each destination then received a score out of 100.
Australia took the top spot as the world's most relaxing destination, scoring 73.8 out of 100.
BookRetreats recognized Australia for offering visitors "space to breathe," which often isn't found in crowded European holiday destinations.
"Key to this ranking is the country's balance of vast natural landscapes and low tourist numbers," stated the travel website.
It also received recognition for its natural spaces, as it is home to over 700 national parks. Australia also offers 4,700 wellness experiences, which added to the list of reasons it came in first place.
Canada received the silver medal with a score of 72.5 and was the only North American destination to make the top 25.
BookRetreats' new ranking of the most relaxing places to visit.
"Nature defines the Canadian travel experience," stated the website. "Home to the world's largest collection of lakes and the mesmerizing aurora borealis, Canada's untouched wilderness is the place for peace seekers."
Canada also topped Australia in wellness experiences, offering 4,724 activities, including thermal springs in the Rockies and silent retreats in eastern Ontario.
Iceland, Finland and New Zealand rounded out the top five spots.
Canada has fared well when it comes to travel rankings this year.
In October, thousands of travellers who participated in the 2024 Condé Nast Readers' Choice Awards named it one of the top countries in the world.
Most recently, Canada came second in Wanderlust magazine's ranking of the world's most desirable countries, just below Australia, which again took first place.
With files from Isabelle Docto
Potifor/Shutterstock
Latest Videos
Latest Videos
Join the conversation Load comments







